Researchers have developed a device that can switch cell function to rescue failing body functions with a single touch. The technology, known as Tissue Nanotransfection (TNT), injects genetic code into skin cells, turning those skin cells into other types of cells required for treating diseased conditions.
Researchers at The Ohio State University Wexner Medical Center and Ohio State’s College of Engineering have developed a new technology, Tissue Nanotransfection (TNT), that can generate any cell type of interest for treatment within the patient’s own body. This technology may be used to repair injured tissue or restore function of aging tissue, including organs, blood vessels and nerve cells.
In a new study published in Nature Nanotechnology, first author Daniel Gallego-Perez of Ohio State demonstrated that the technique worked with up to 98 percent efficiently.
"It takes just a fraction of a second. You simply touch the chip to the wounded area, then remove it."
“By using our novel nanochip technology, injured or compromised organs can be replaced. We have shown that skin is a fertile land where we can grow the elements of any organ that is declining,” said Dr. Chandan Sen, director of Ohio State’s Center for Regenerative Medicine & Cell Based Therapies, who co-led the study with L. James Lee, professor of chemical and biomolecular engineering with Ohio State’s College of Engineering in collaboration with Ohio State’s Nanoscale Science and Engineering Center. Researchers studied mice and pigs in these experiments. In the study, researchers were able to reprogram skin cells to become vascular cells in badly injured legs that lacked blood flow. Within one week, active blood vessels appeared in the injured leg, and by the second week, the leg was saved. In lab tests, this technology was also shown to reprogram skin cells in the live body into nerve cells that were injected into brain-injured mice to help them recover from stroke.
“It takes just a fraction of a second. You simply touch the chip to the wounded area, then remove it,” said Chandan Sen, PhD, director of the Center for Regenerative Medicine and Cell-Based Therapies at The Ohio State University Wexner Medical Center. “At that point, the cell reprogramming begins.”
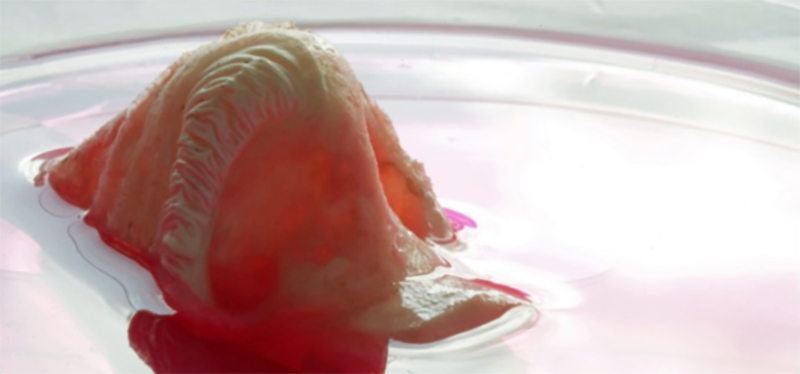
In a series of lab tests, researchers applied the chip to the injured legs of mice that vascular scans showed had little to no blood flow. “We reprogrammed their skin cells to become vascular cells,” Sen said. “Within a week we began noticing the transformation.” By the second week, active blood vessels had formed, and by the third week, the legs of the mice were saved—with no other form of treatment.
“It extends the concept known as gene therapy, and it has been around for quite some time,” said study collaborator James Lee, PhD, a professor of chemical and biomolecular engineering at Ohio State. “The difference with our technology is how we deliver the DNA into the cells.”
The nanochip, loaded with specific genetic code or certain proteins, is placed on the skin, and a small electrical current creates channels in the tissue. The DNA or RNA is injected into those channels where it takes root and begins to reprogram the cells.
Related articles
“What’s even more exciting is that it not only works on the skin, but on any type of tissue,” Sen said. In fact, researchers were able to grow brain cells on the skin surface of a mouse, harvest them, then inject them into the mouse’s injured brain. Just a few weeks after having a stroke, brain function in the mouse was restored, and it was healed. Because the technique uses a patient’s own cells and does not rely on medication, researchers expect it to be approved for human trials within a year. “This is difficult to imagine, but it is achievable, successfully working about 98 percent of the time. With this technology, we can convert skin cells into elements of any organ with just one touch. This process only takes less than a second and is non-invasive, and then you're off. The chip does not stay with you, and the reprogramming of the cell starts. Our technology keeps the cells in the body under immune surveillance, so immune suppression is not necessary,” said Sen, who also is executive director of Ohio State’s Comprehensive Wound Center.
TNT technology has two major components: First is a nanotechnology-based chip designed to deliver cargo to adult cells in the live body. Second is the design of specific biological cargo for cell conversion. This cargo, when delivered using the chip, converts an adult cell from one type to another, said first author Daniel Gallego-Perez, an assistant professor of biomedical engineering and general surgery who also was a postdoctoral researcher in both Sen’s and Lee’s laboratories.
TNT doesn’t require any laboratory-based procedures and may be implemented at the point of care. The procedure is also non-invasive. The cargo is delivered by zapping the device with a small electrical charge that’s barely felt by the patient.
“The concept is very simple,” Lee said. “As a matter of fact, we were even surprised how it worked so well. In my lab, we have ongoing research trying to understand the mechanism and do even better. So, this is the beginning, more to come.”